Archive for the ‘medicine’ Category

AJGpr client, Dr. Norman Marcus, author of End Back Pain Forever: A Groundbreaking Approach to Eliminate Your Suffering and founder of The Norman Marcus Pain Institute, recently posted a blog about the growing problem of prescription drug addiction and misuse and what government is doing about it. Here it is.
49 States Adopt Prescription Drug Database to Prevent Prescription Drug Abuse by Dr. Norman Marcus
Because of the growing problem of addiction, misuse, and diversion, 49 states have now adopted a state prescription drug database. You may have read an article recently in The New York Times about Missouri being the only state that has not adopted such a database. In New York, as a prescriber of controlled substances, each time a patient is prescribed any type of controlled substance, I must log into the NYS website to confirm that a patient is not receiving other medications from other doctors.
I found a few patients who had not been honest with me and had received medications from other doctors. Unfortunately, the small occurrence of dishonest behavior has obliged all doctors to be alert for the possible misuse of medication. At the Norman Marcus Pain Institute, I implement several rules for patients receiving any type of controlled substance from me. Here are a few of them:
• Only one physician can prescribe all pain medications.
• Only one pharmacy should be used to obtain all pain related medications.
• All medications, including herbal remedies and over the counter medications, need to be reported since all medications can interact with one another.
• Medications must be kept in a safe and secure place, such as a locked cabinet or safe.
Following these simple rules will help protect my patients and their families from improper use of pain medication.
AJGpr client, Dr. Norman Marcus, author of End Back Pain Forever: A Groundbreaking Approach to Eliminate Your Suffering and founder of The Norman Marcus Pain Institute, recently posted a blog entitled http://www.normanmarcuspaininstitute.com/49-states-adopt-prescription-drug-database-to-prevent-prescription-drug-abuse/ Tennis Elbow Causing Your Pain? PRP is NOT the Solution Study Shows.
In this blog he talks about what treatments work to end tennis elbow pain and what don’t. Below is his post.
——————————————————————————————————————————————
Tennis Elbow Causing You Pain? PRP is NOT the Solution Study Shows
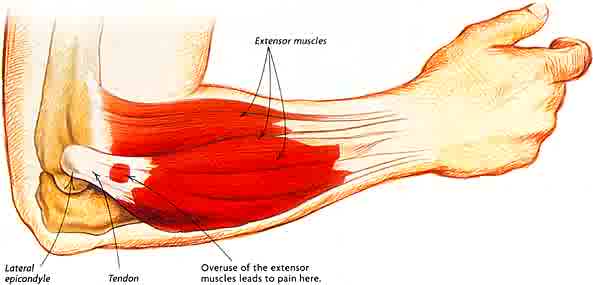
At NMPI, we frequently see patients in our office with pain in their elbow. Most often it’s tennis players who complain of persistent pain in the forearm as the result of overuse from racquet sports but other sports and non-athletic activities can also put you at risk for this condition known as Tennis Elbow (TE), or lateral epicondylitis. Strain related changes in the tendons that join the forearm muscles to the outside of the elbow can be very painful.
I was not surprised to read in the British Journal of Sports Medicine, that a recent study (Strong Evidence Against Platelet-rich Plasma Injections for Chronic Lateral Epicondylar Tendinopathy: A Systematic Review) reported that PRP, which I recently reported as not being effective for hamstring injuries, is now found to be ineffective for persistent Tennis Elbow as well. PRP has been increasingly used for many painful conditions that athletes experience. This is based on the finding that in laboratory animals healing can be induced in damaged tissue if platelets are injected into the injured area. The popularity of PRP for TE has growndespite no strong evidence that it actually works. Sir William Osler, a renowned physician once said “use every new treatment as quickly as possible before it stops working.” At NMPI, we do not rush to use a “new” approach just because it is new. We are committed to eliminating our patients’ pain and preventing its recurrence.
TE is commonly diagnosed by producing pain when pressing on the tendons that attach to the lateral epicondyle along with pain when the wrist is pulled upward (dorsiflexion) against resistance. TE is generally self-limiting but in some patients it may take more than a year to get better with no treatment. When the pain and tenderness persist various treatments have been tried.
Here’s what works:
- In a 2010 paper, an exercise treatment was found to be very effective in relieving TE pain and tenderness.
- At NMPI, we treat these tender muscles successfully with a laser or with muscle injections.
Here’s what doesn’t work:
- Steroids are not recommended since there is no inflammation in TE and steroids can actually damage the tendon.
- PRP for tennis elbow has been found to not be effective
Newer treatments are often not better. It is always best to first treat any lasting pain problem with the least invasive, safest, and least expensive interventions. This is called the step-care model and the approach you will receive at the Norman Marcus Pain Institute.
DID YOU KNOW THAT…
- 4 out 5 Americans suffer from back pain.
- Back pain, now the most common disability in the United States, is the number one reason people go to the doctor or miss work.
- In fact, every year nearly 12 million Americans make new-patient visits to physicians for back pain and one hundred million visit chiropractors.
WELL…
A few weeks ago, The NewYork Times, published an article entitled, Common Back and Leg Pain Treatment May Not Help Much, Study Says. Basically, the article talks about a study recently published in the New England Journal of Medicine that shows the common and widely used treatment for lower back and leg pain caused by stenosis — a stenosis injection which combines a steroid and a local anesthetic is INEFFECTIVE. In fact, the article goes on to say doctors and patients should think twice about using the treatment at all.
AJGpr client, Dr. Norman Marcus, one of the nation’s leading specialists and a pioneer in the treatment and relief of chronic pain, and author of End Back Pain Forever: A Groundbreaking Approach to Eliminate Your Suffering, has been saying this for YEARS!
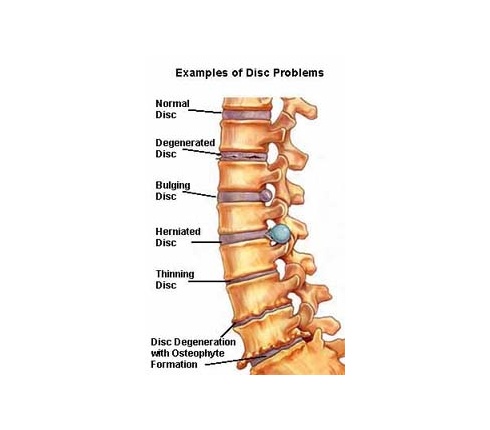
Dr. Marcus contends that, “One reason why this approach is ineffective is that the pain in the back and leg may not be the result of the narrowing or other supposed abnormalities seen on the MRI or CT scan. It is well known that very few (in one published article – less than 10%) scans of the low back in adults are read as normal; as many as 40% of adults with no back pain have herniated discs, and 70% have degenerated discs.”
Named one of the “Best Doctors in New York for pain management” by New York Magazine and founder of the Norman Marcus Pain Institute, Dr. Marcus responded to the The New York Times article and the New England Journal of Medicine study in his blog Epidural steroids are not effective for spinal stenosis.
——————————————————————————————————————————————
Epidural steroids are not effective for spinal stenosis.
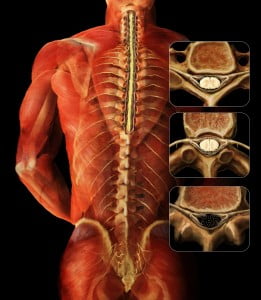
I have been suggesting for many years that there is an overuse of spinal injections and surgeries for low back and leg pain, so it was no surprise when I read an article in The New York Times (NYT) that reported on a study recently published in the New England Journal of Medicine[1] about patients with spinal stenosis who are frequently treated with a procedure that has been shown to be ineffective. Epidural steroid and lidocaine injections for patients found to have spinal stenosis were no better than epidural injections of lidocaine alone. In chapter 4 of my book End Back Pain Forever I discuss the many reasons for back pain. MRIs and CT scans of the low back will almost always find something such as spinal stenosis or a degenerated or herniated disc even in patients without pain. Therefore the US Institute of Medicine suggests that these imaging studies should not be done routinely since what you find in the study is frequently not the cause of your pain. The most common cause of back pain is muscles and other soft tissue. If you treat the diagnosis you got from the MRI or CT and the actual reason for the pain is muscle, it makes sense that the treatment will frequently fail, which it does!
The NYT report of this relatively large, randomized, double blind, controlled study clearly demonstrates the ineffectiveness of the use of steroids for symptoms attributable to spinal stenosis (narrowing of the canal in the spine which contains the spinal cord) which occurs frequently as we age. The treatments most often provided are epidural steroids to theoretically reduce the inflammation of the nerves being squeezed by the narrow canal, and surgery to widen the canal. Both approaches have a significant failure rate.
At the Norman Marcus Pain Institute we have shown in multiple published articles that one reason why these approaches are ineffective is that the pain in the back and leg may not be the result of the narrowing or other supposed abnormalities seen on the MRI or CT scan. It is well known that very few (in one published article- less than 10%) scans of the low back in adults are read as normal; as many as 40% of adults with no back pain have herniated discs, and 70% have degenerated discs. So it is “normal” to find an abnormality.
Our unique physical examination, utilizes an instrument I developed, reveals that many patients with back and leg pains have areas of muscle tenderness that are the source of their pain yet are overlooked. One study of more than 23,000 patients[2] found that 70-80% of patients with back pain were diagnosed with sprains and strains of muscle and other soft tissue. It’s hard to believe then, armed with this knowledge, that muscle examination and treatment is not part of the typical standard of care for back pain in the USA[3]. If we are to properly address the cause of most back pain, the evaluation and treatment of its muscular causes must be addressed.
[1] Friedly JL, Comstock BA, Turner JA, et al. A Randomized Trial of Epidural Glucocorticoid Injections for Spinal Stenosis. New England Journal of Medicine. 2014:374:11-21.
[2] Deyo RA, Weinstein JN. Primary care – low back pain. New England Journal of Medicine. 2001:5:363-70.
[3] Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, et al. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.